As part of the adjudication process, claims are either approved, denied, or require more information. This results in a range of manual tasks which must occur to manage appeals from patients or providers, investigations, and administration of denials — creating a cost center within the revenue management cycle.
Instabase for Appeals and Denials
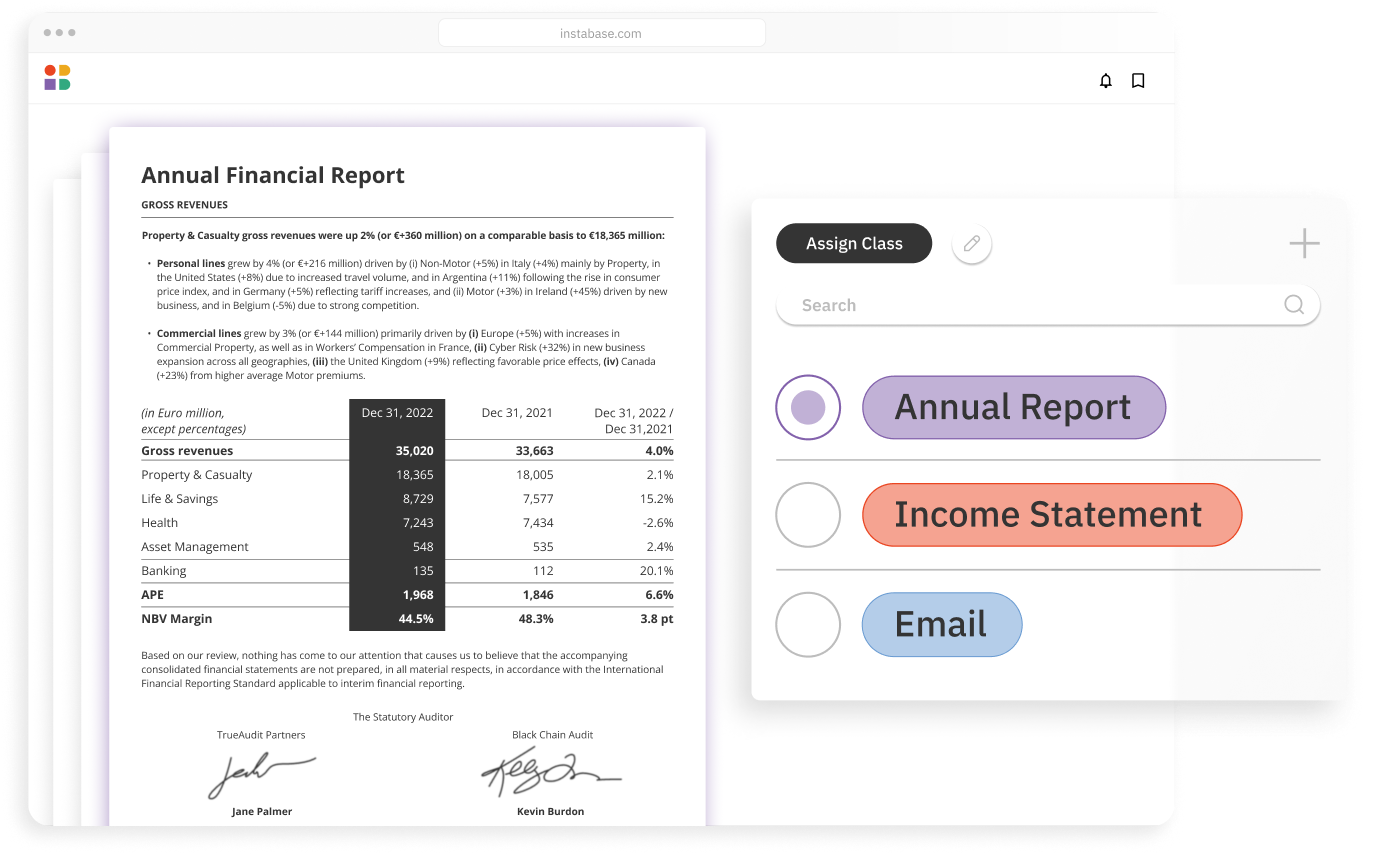
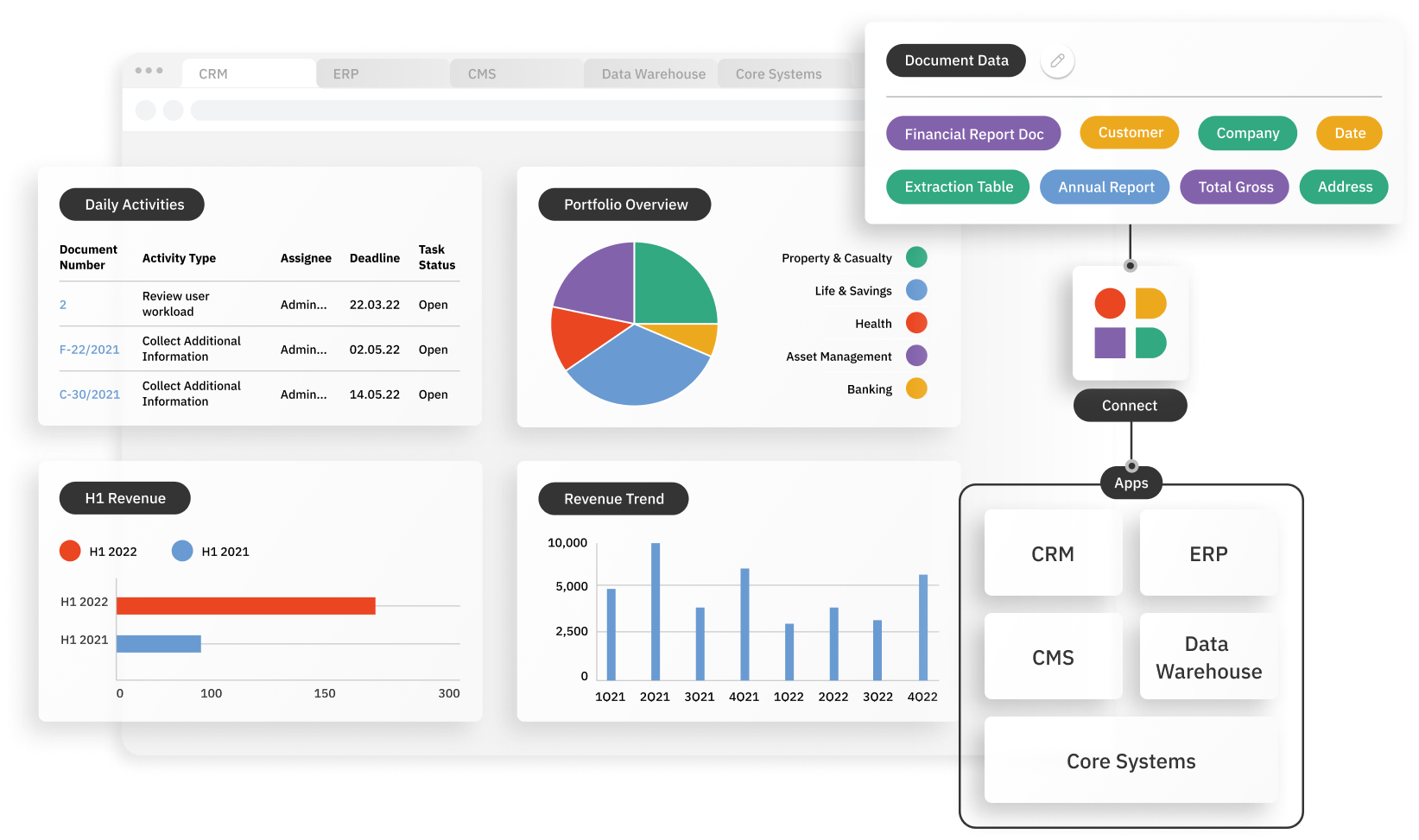
Instabase automates document understanding for all documents included in the appeals and denials process, regardless of document type or format, to streamline an end-to-end workflow.

Processing Appeals and Denials
Why Instabase?
The Instabase Automation Platform for Unstructured Data helps health insurance payors during the adjudication process by leveraging deep learning for document understanding, increasing accuracy, and reducing processing time.
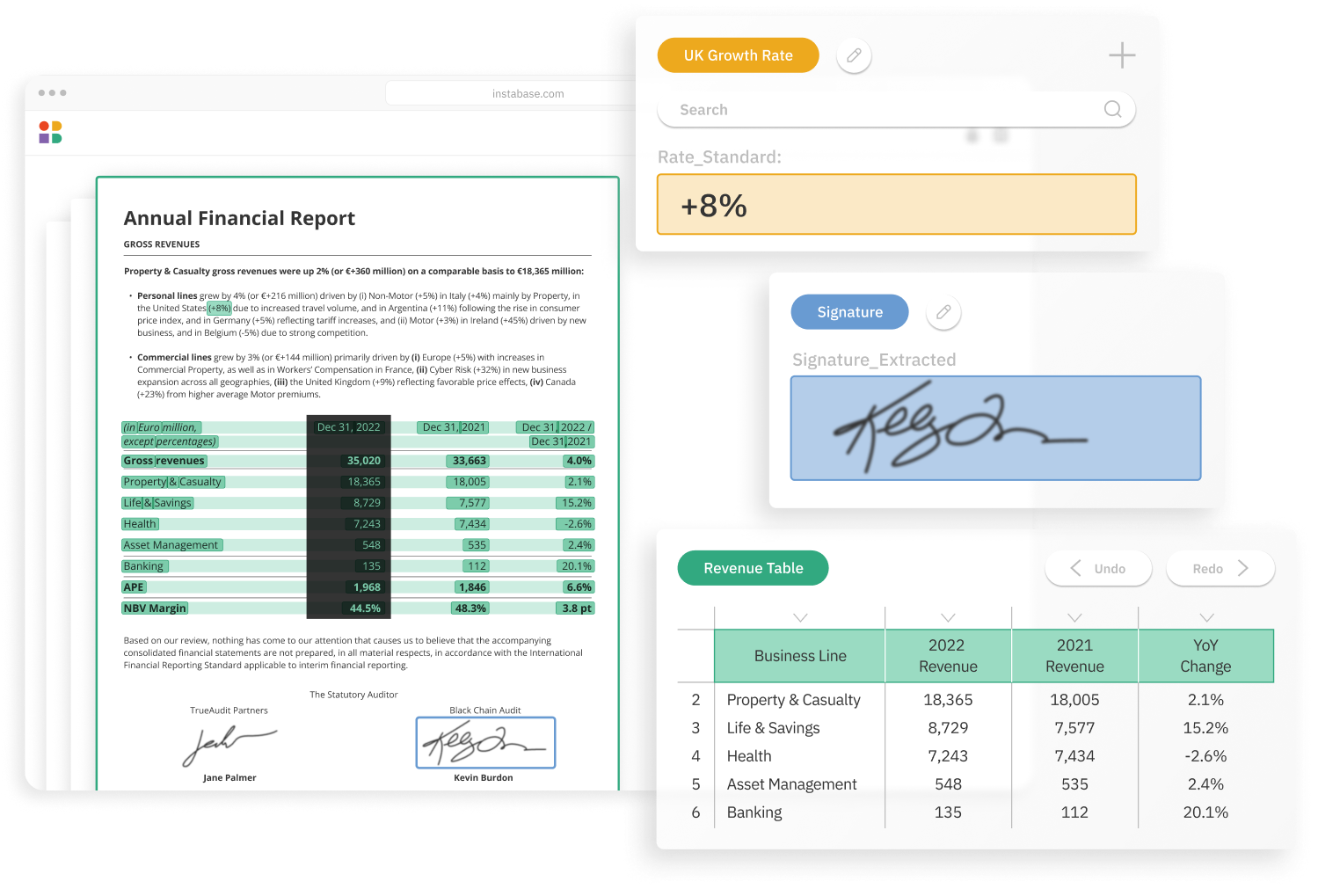
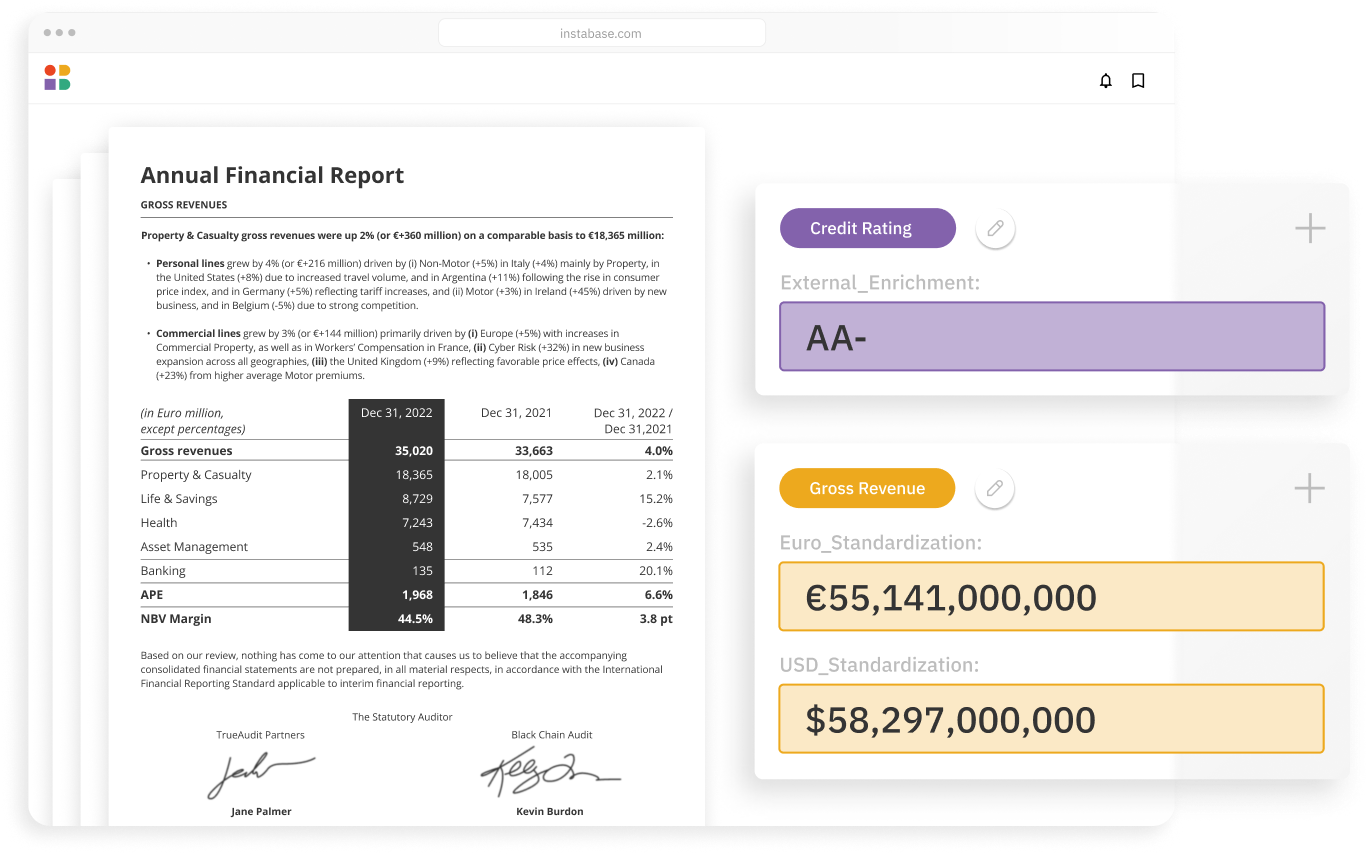
Unlock unstructured data that others can’t
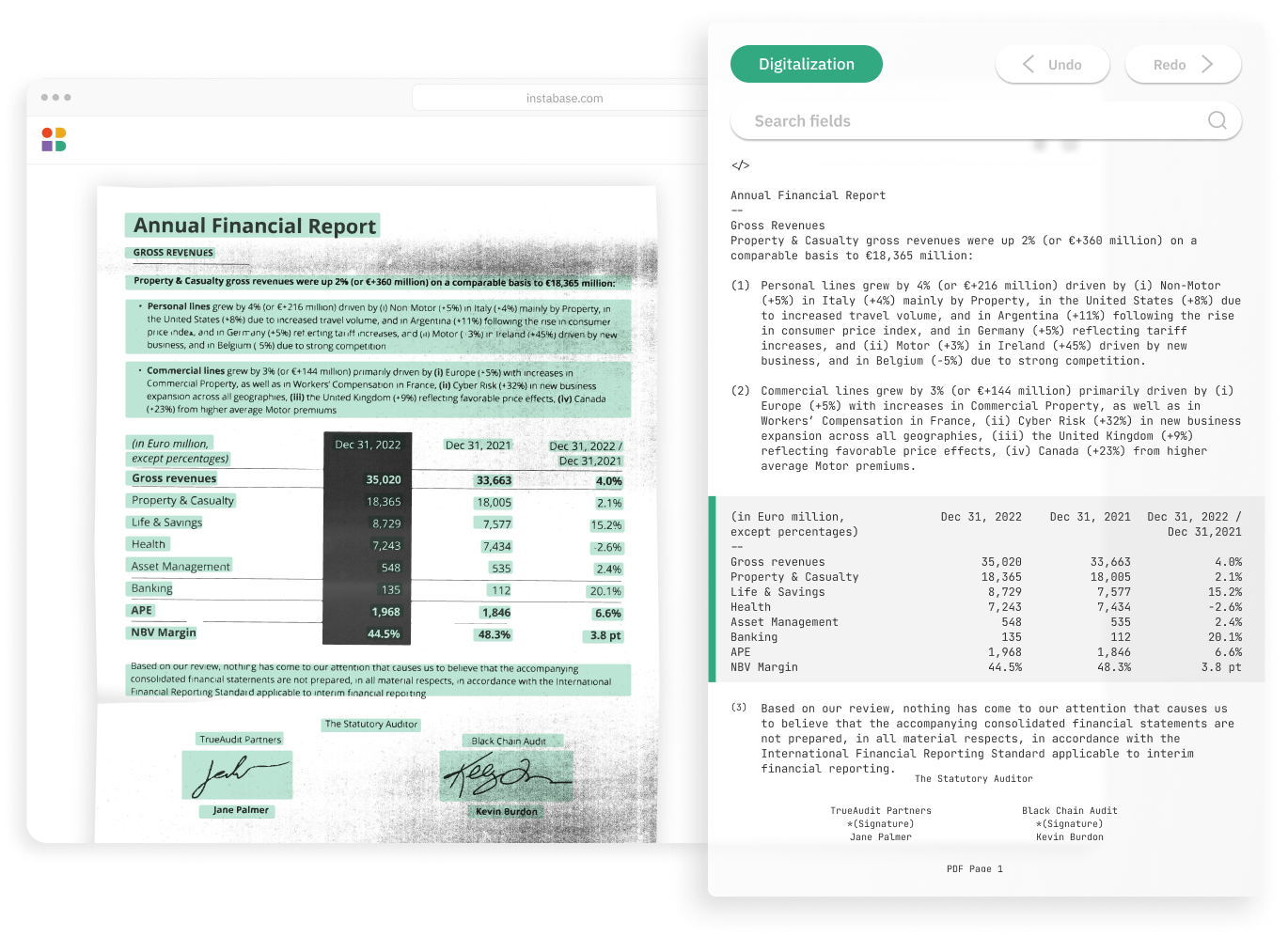
Understand your most complex documents with the latest in AI from Instabase and the broader market
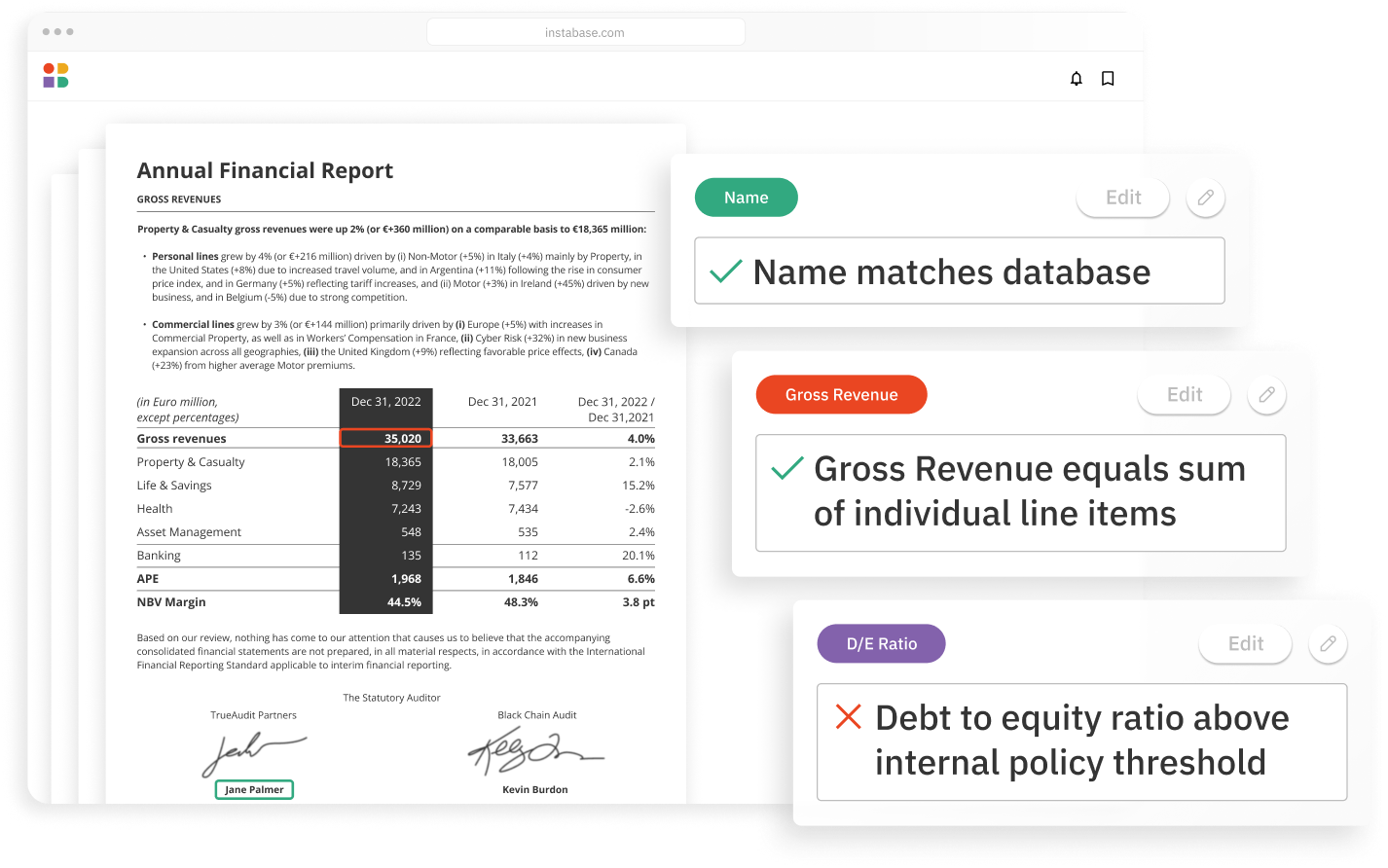
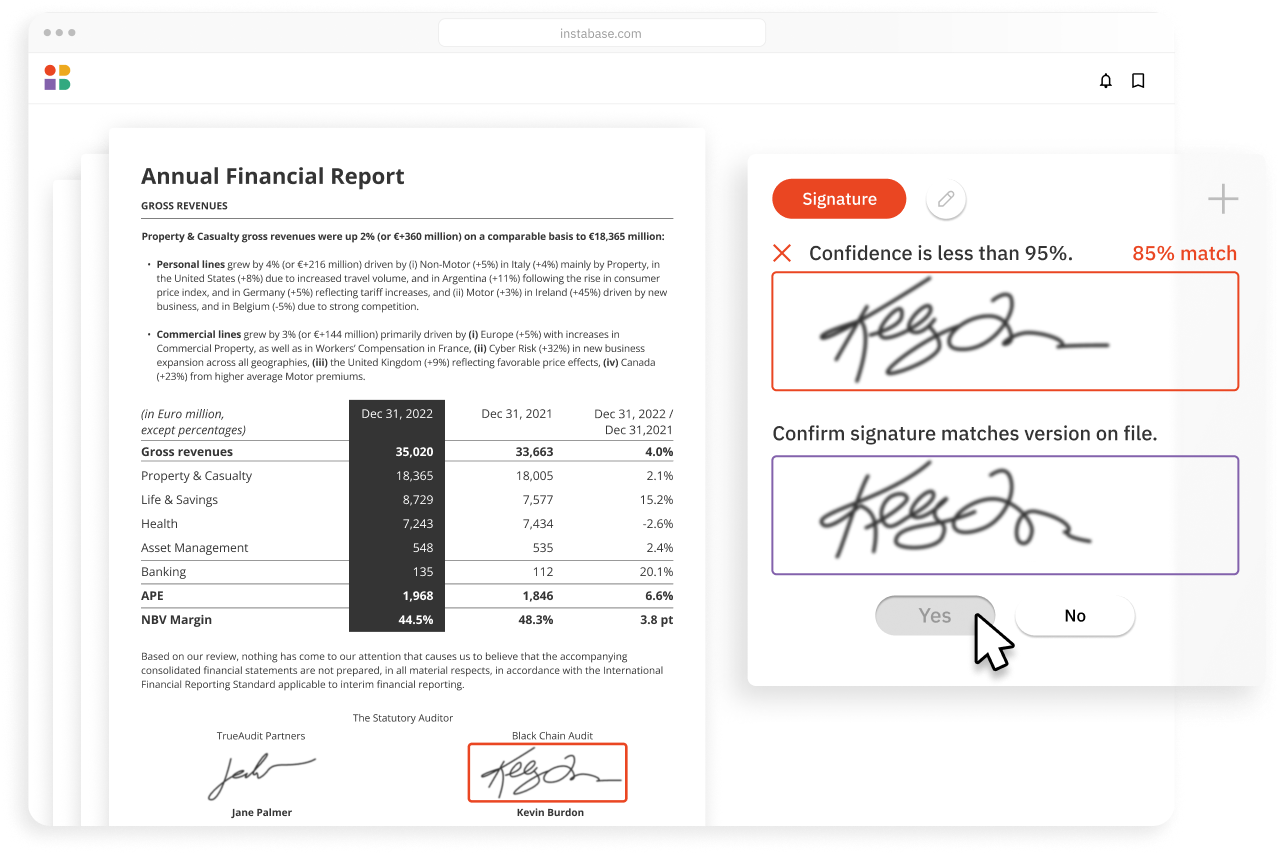
Achieve unrivaled automation & accuracy
Minimize errors and boost automation with an extensive suite of validations and business logic
Build solutions 10x faster
Launch end-to-end solutions in days with low code building blocks for every step in your workflow
How it works
Instabase combines the most powerful technologies for every step of the process, so you can automatically understand any document in the submissions process.