Utilization Management prevents fraud by assessing the cumulative usage of healthcare plans by patients. This analysis typically happens as part of claims adjudication, either to proactively or retrospectively prevent misuse or overpayment.
Instabase for Utilization Management
Instabase automates document understanding of all relevant documents for healthcare plan usage, streamlining utilization management in an end-to-end workflow.

Managing Healthcare Plan Utilization
Why Instabase?
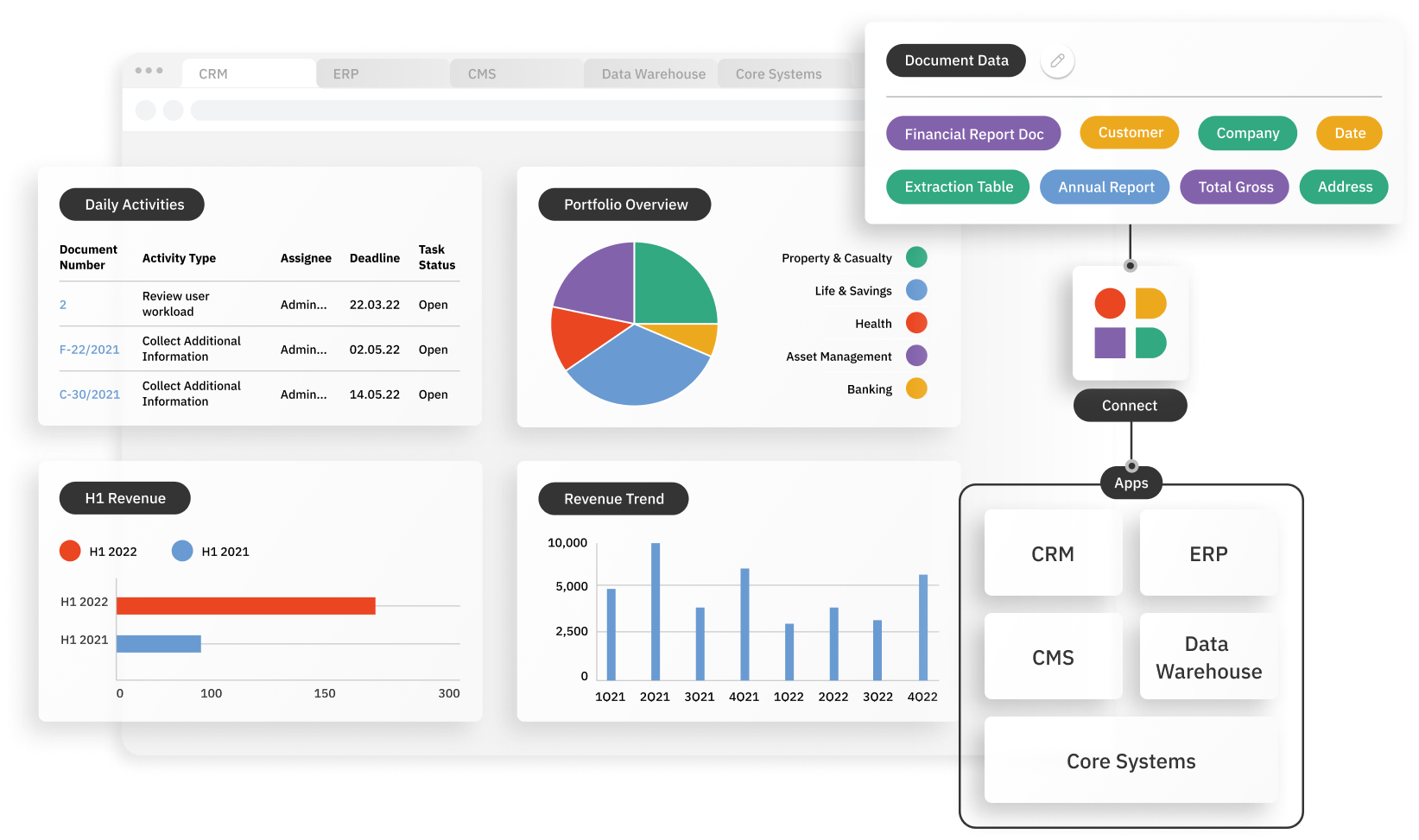
The Instabase Automation Platform for Unstructured Data uses deep learning and natural language processing technology to help health insurance payors with utilization management by increasing accuracy and reducing processing times.
Unlock unstructured data that others can’t
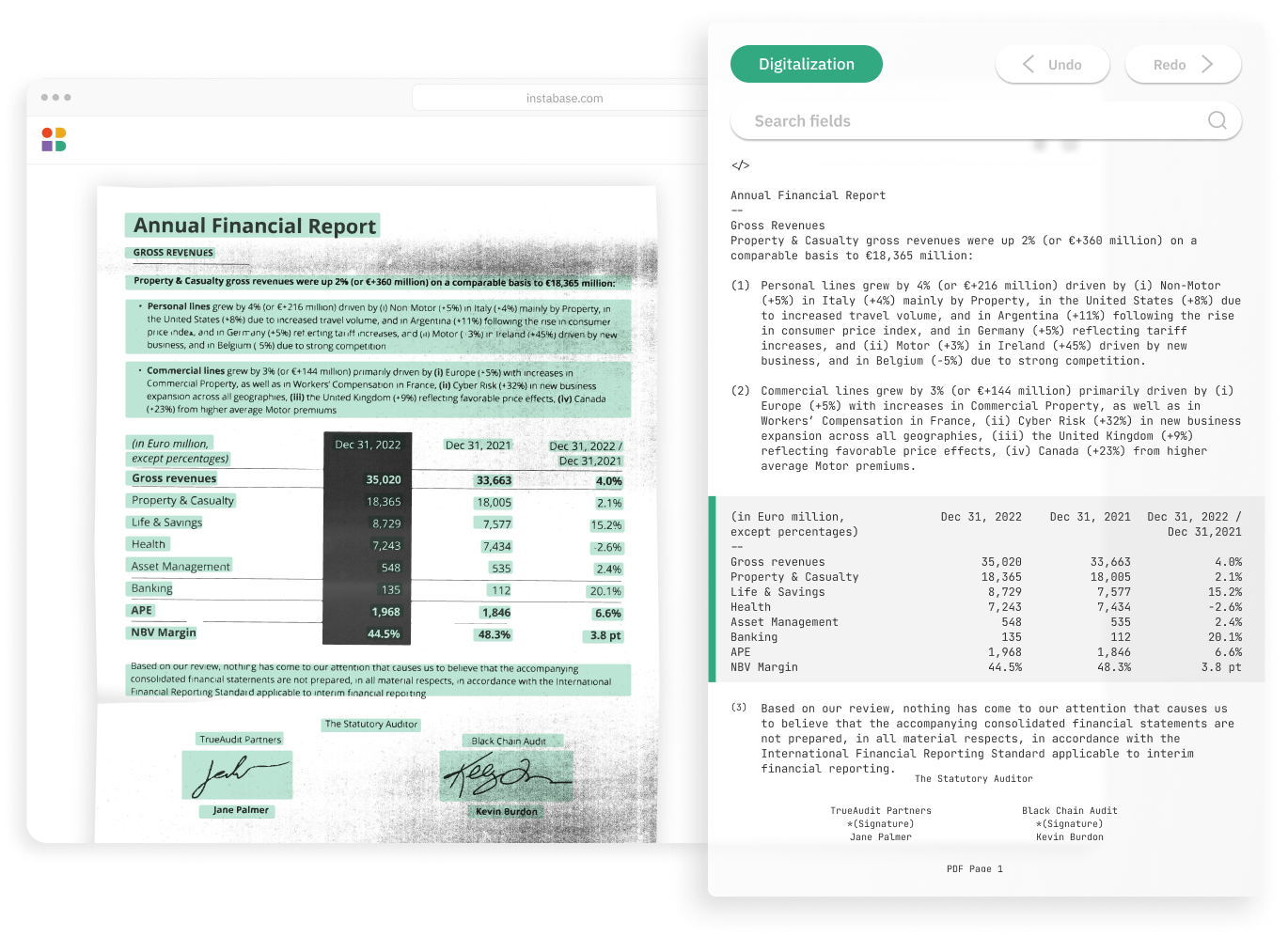
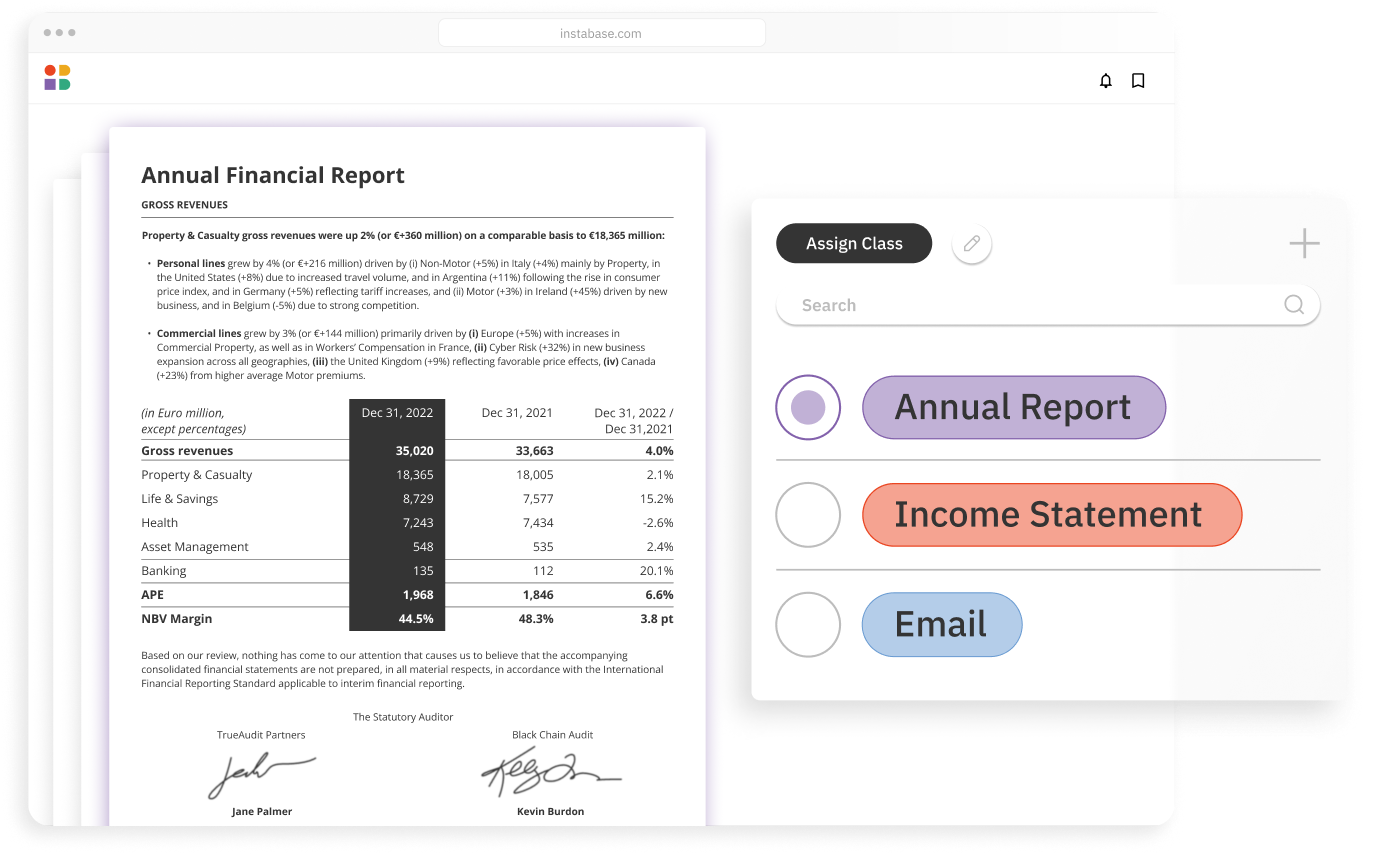
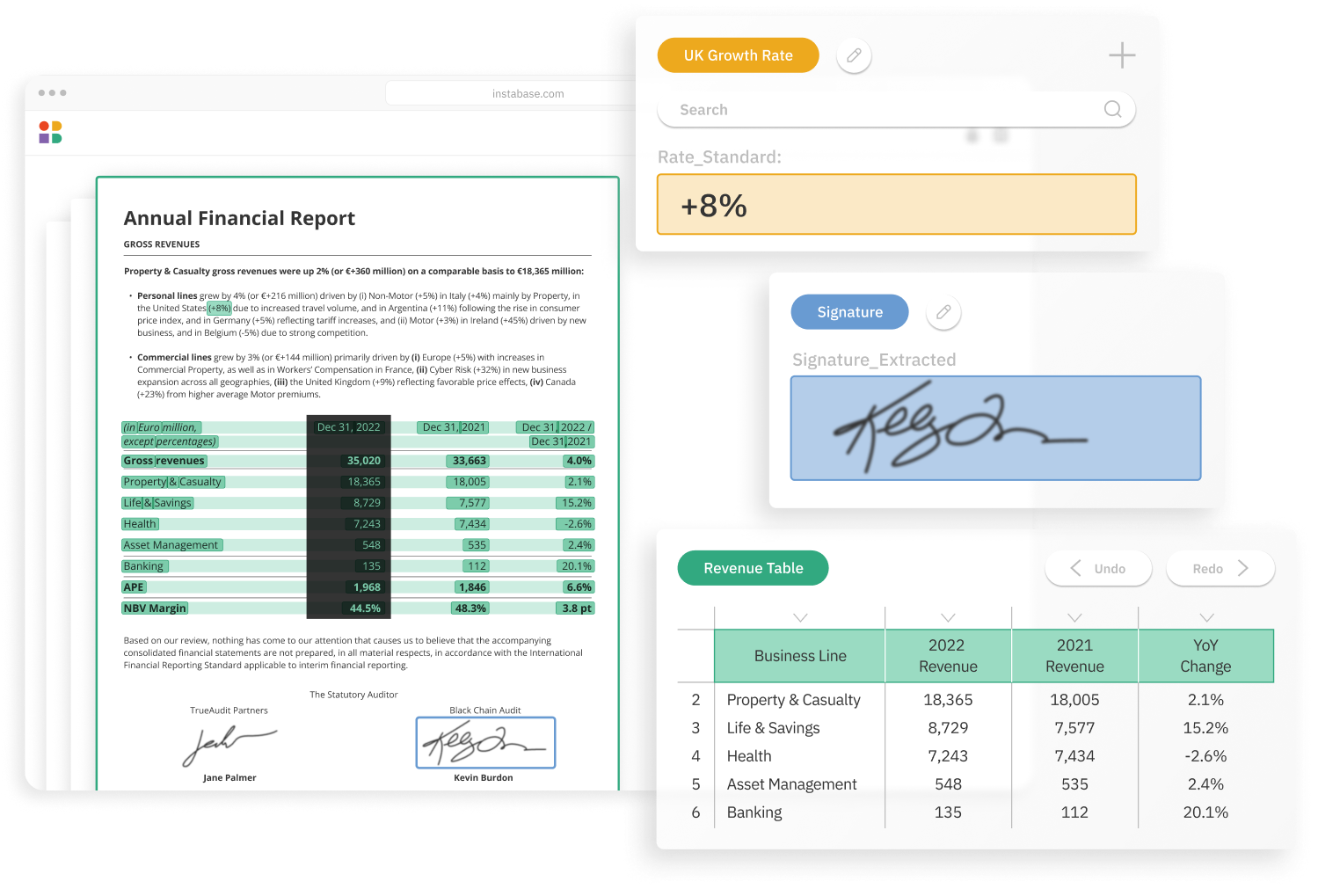
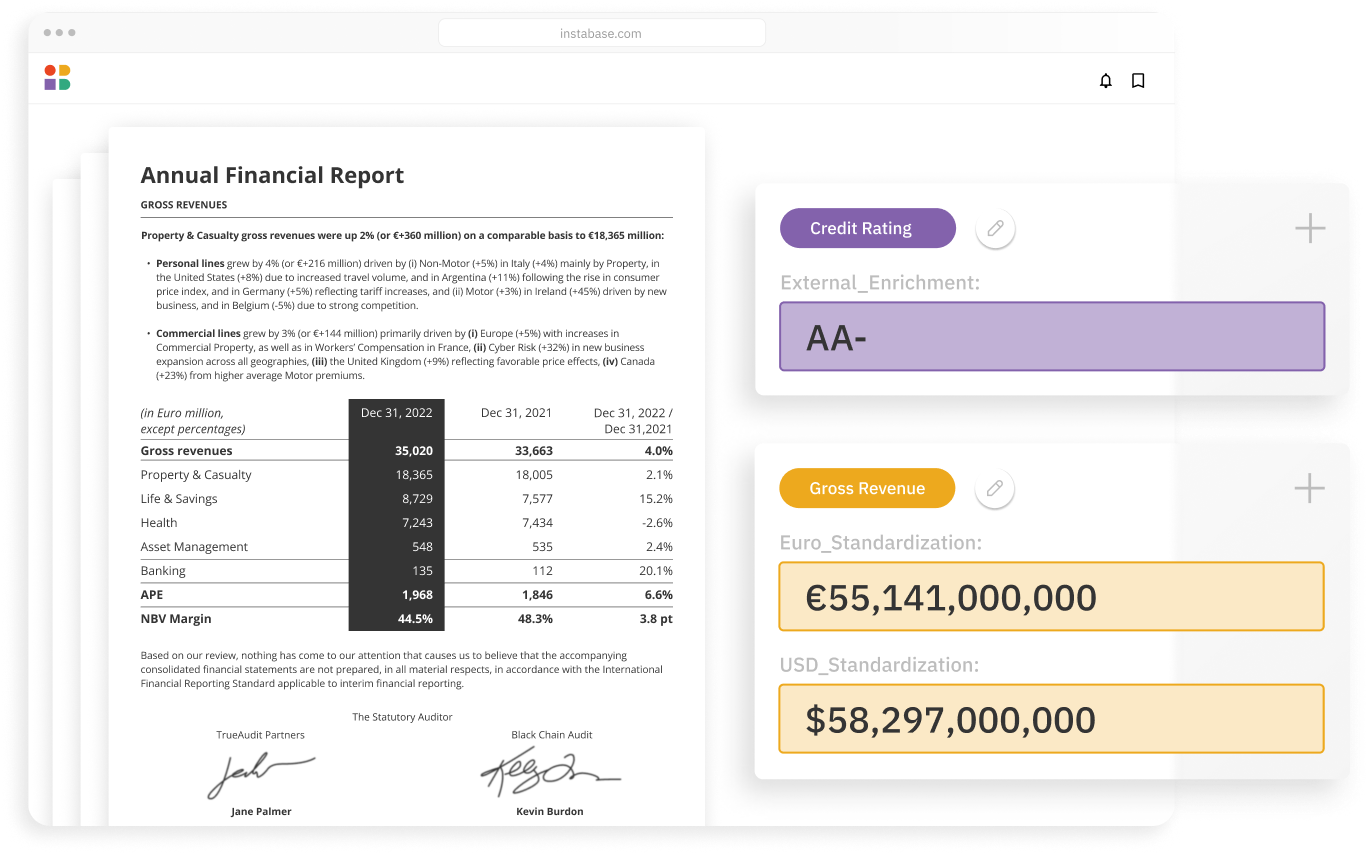
Understand your most complex documents with the latest in AI from Instabase and the broader market
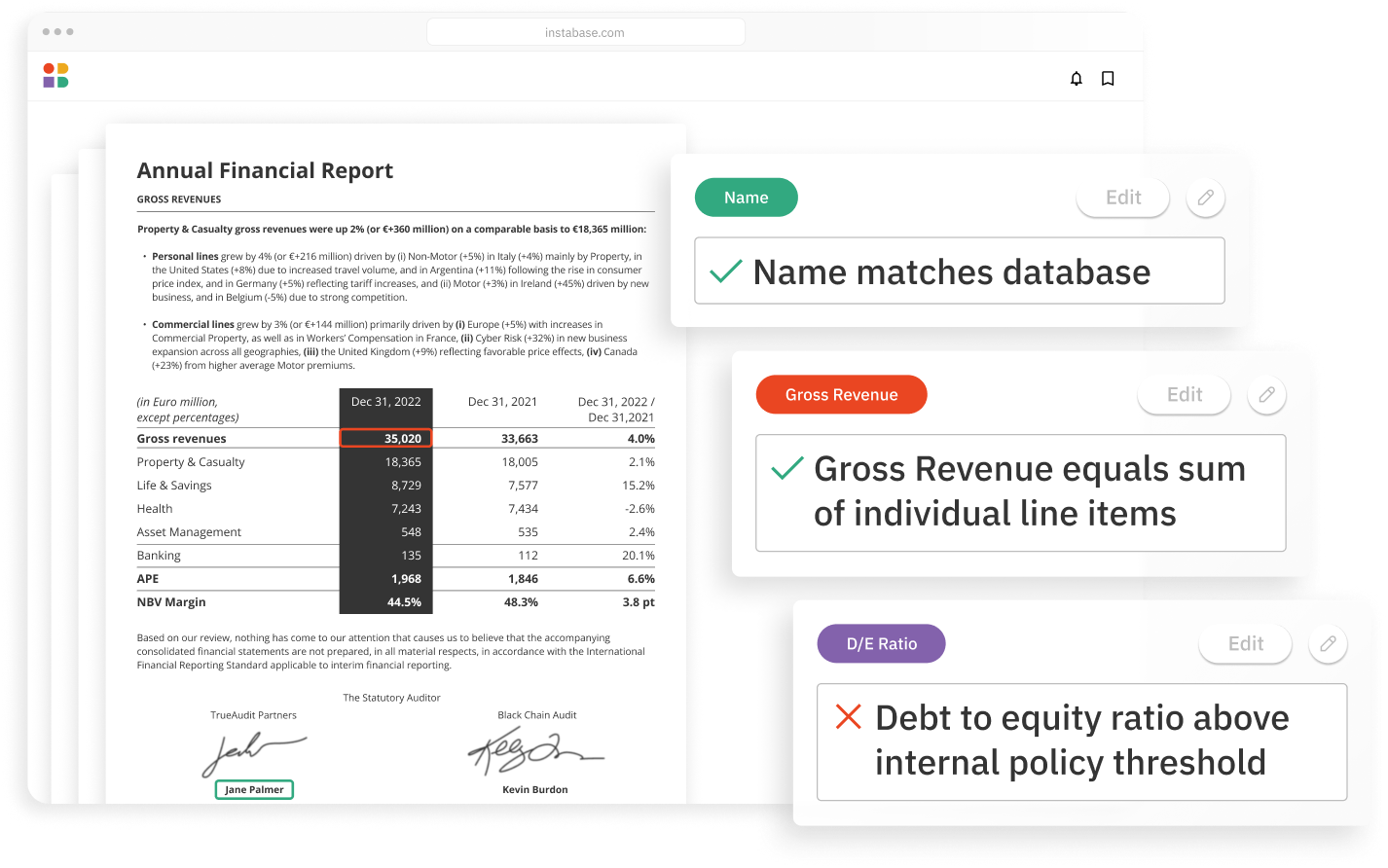
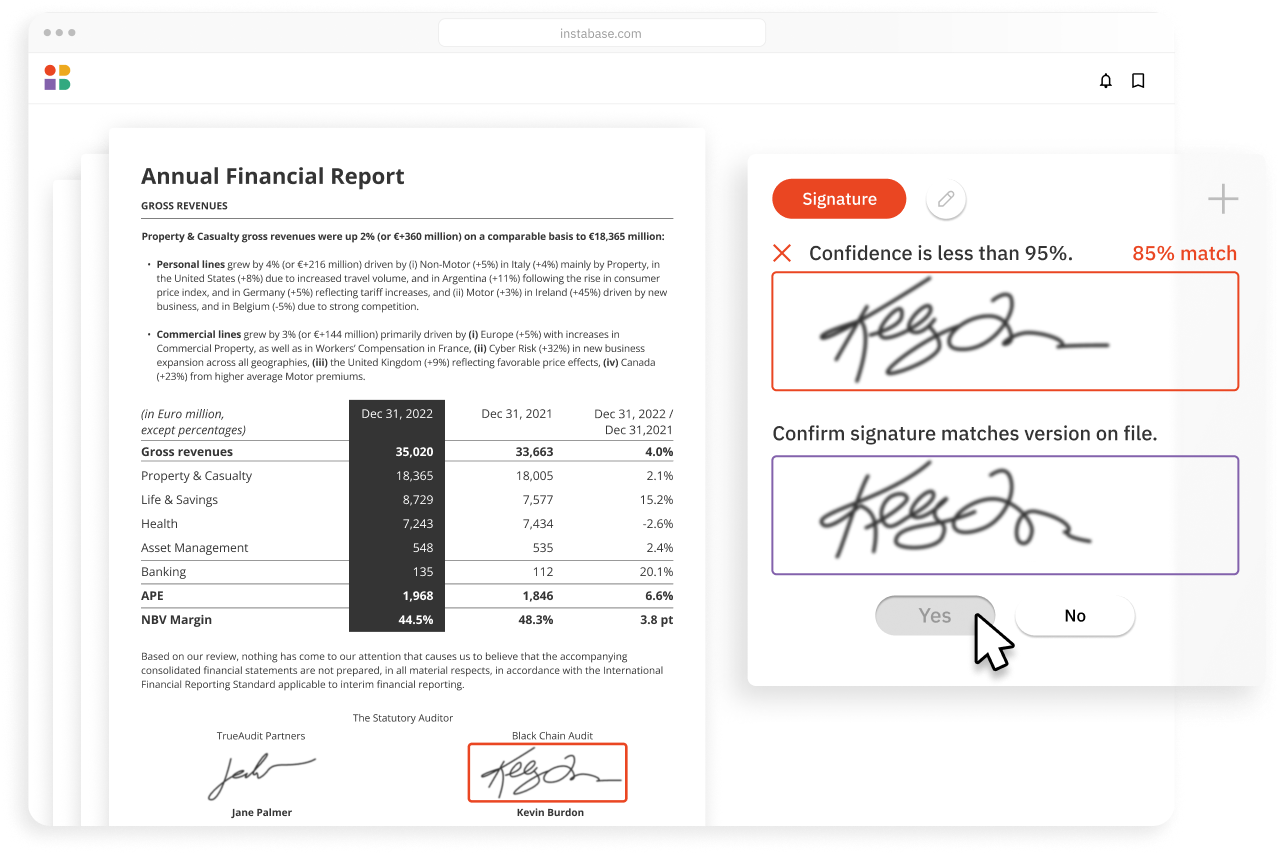
Achieve unrivaled automation & accuracy
Minimize errors and boost automation with an extensive suite of validations and business logic
Build solutions 10x faster
Launch end-to-end solutions in days with low code building blocks for every step in your workflow
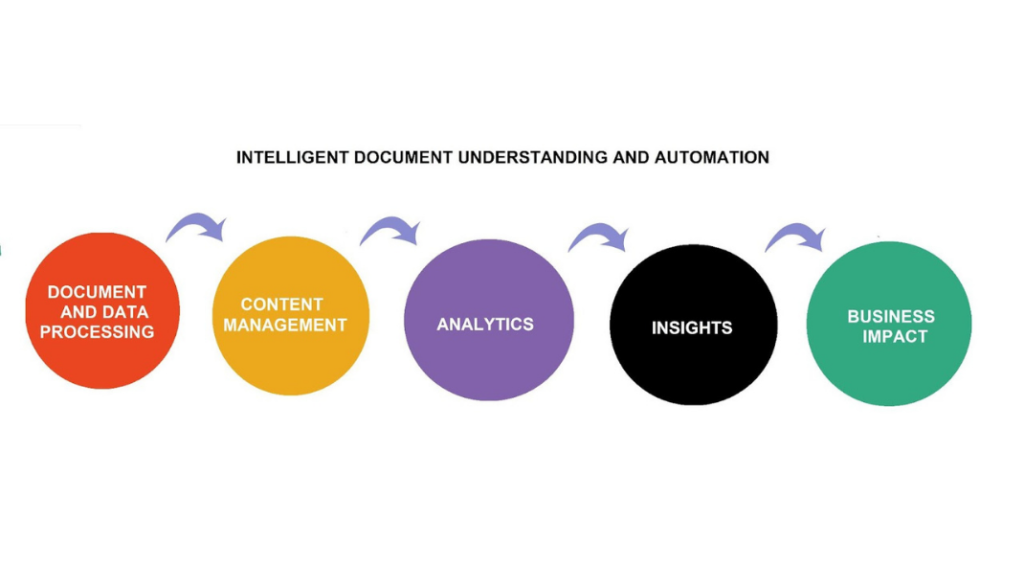
How it works
Instabase combines the most powerful technologies for every step of the process, so you can automatically understand any document in the submissions process.